BLOCKCHAIN TECHNOLOGY USING ARTIFICIAL INTELLIGENCE FOR CARDIOVASCULAR MEDICINE
INTRODUCTION
Artificial intelligence (AI) is a fast evolving computer science that can categorize and forecast complicated data. AI has achieved considerable success in voice, facial, and image recognition, gaming, and a variety of industrial and scientific sectors, and is now being used to health care. AI can assess heart function from imaging, estimate cardiac rhythm and function from the electrocardiogram (ECG), and make some clinical judgments much like specialists in cardiovascular medicine.
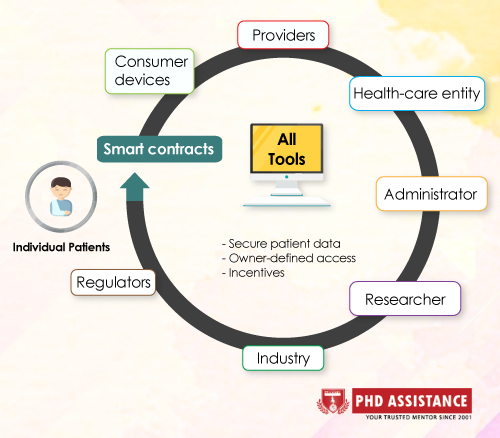
However, AI’s potential to enable customised cardiovascular treatments by identifying novel phenotypes beyond established illness syndromes, enhancing outcome forecasts, and personalising medication is largely unfulfilled. Despite the fact that AI appears to be on the verge of realising this ideal of precision medicine, especially with the development of wearable sensors and omic technologies, progress has been uneven. The scarcity of big, secure, diverse, and granular data sets with reliable follow-up across wide, at-risk groups is a serious obstacle. This issue is becoming more widely acknowledged as a barrier to AI in cardiovascular care. Blockchain allows for a significant conceptual leap by allowing ‘incentives’ to flow to the owner of any data element based on its value. This partnership may pave the way for a health-related cryptocurrency with far-reaching consequences. Incentives might be offered not just to the owner of the original data (genetic, blood, or ECG), but also to clinicians whose efforts result in a diagnosis or better results. Similarly, administrators who enhance patient outcomes or resource use might be rewarded. Incentives for research might be directed to data owners who assist Researchers or who manage a valuable database, or to creators of effective analysis methods.
INTEGRATION OF BLOCKCHAIN WITH AI
Blockchain technology has the potential to speed up the development of data-hungry AI applications. Convolutional neural networks, for example, were recently trained on ECGs from a single wearable monitor in 53,549 individuals and gave cardiologist-level diagnosis accuracy for arrhythmias3. However, several arrhythmias were under-represented in that data source, and the results may change if different data sets were utilised. A blockchain-enabled data marketplace may make secure data integration from other vendors or health-care systems easier, allowing for more instances of particular arrhythmias in the data set and therefore better training. As a result, various different techniques for integrating blockchain with AI are being considered.
The use of blockchain to standardise health-data formats for AI training, clinical trials, and regulatory reasons is a logical fit. Data from various cardiovascular sources, such as portable ECG monitors, other wearable devices, current hospital-based electronic medical records, biobanks, and non-medical data, such as activity logs, social media, or e-mail threads, is becoming increasingly difficult to combine. This problem has a scalable answer in blockchain.
Blockchain enables the tracing of different block (record) types and the dissection of granular data. If the data from the TOPCAT trial had been obtained using blockchain, the regional differences in the outcomes could have been easily monitored. Given documented disparities in drug metabolism or illness propensity between geographical areas, genetic groupings, or other population variances, partitioning data in this way is important and rising in relevance for AI applications and precision health.
The proposed health cryptocurrency model might encourage the submission of uncommon data, which is frequently underrepresented in single-center research or even big registries. Underrepresented racial groupings, geographical locations, and unusual situations are examples. As a result, blockchain-based AI might help to speed up the determination of orphan disease phenotype-specific outcomes, increase the representation of ethnic minorities, and minimise sex-specific inequalities.
CURRENT APPLICATIONS
Several applications that combine blockchain and AI are gaining traction. The American Heart Association has collaborated with the Open Health Network to create AI and blockchain solutions like PatientSphere, a blockchain-based, HIPAA-compliant data-sharing platform that utilises AI to offer treatment plans and exercise tips8. In general, start-up businesses focus on three key areas. First, to utilise blockchain to store data for the creation of an AI model that analyses demographics, cardiac imaging, and other inputs to forecast occurrences such as acute myocardial infarction, and Second, AI algorithms and data should be decentralised. Collaboration between the MedStar Health Research Institute and ObEN, for example, monitors patients with heart failure and rewards those who engage in health-giving behaviours. Third, to employ blockchain as the backbone for an AI-connected network of sensors to anticipate cardiovascular illness, such as Farasha Labs’ or the HealthSync diabetic data trust’s projects.
CHALLENGES TO WIDESPREAD USE
Integration of blockchain with AI is fraught with difficulties. Blockchain solutions in health care must first and foremost be safe. Given the fact that no system is entirely safe, interest in storing sensitive data on an immutable blockchain may be limited. Ethical concerns around AI-blockchain integration may potentially be a factor. Although stakeholders’ identities are kept confidential, public access to medical data on a blockchain ledger isn’t always desired.
Medical data, in general, should not be made public; instead, only the list of encrypted transactions or blocks holding access permissions to the data should be made public; medical data would then be stored on dispersed servers. A so-called 51 percent assault, in which a hostile person gains majority controls, may potentially make blockchain susceptible. This has been observed in the Bitcoin network, where four mining pools supply the majority of the computing power. Although health-care firms are unlikely to be malevolent, they are likely to provide more than 51% of hashes. Finally, data security, scalability, data integrity, ethics, and computing resources will all be addressed by consensus and professional society standards and regulators.
CONCLUSIONS
By greatly increasing the availability of Data for AI Development and training, sharing proprietary AI algorithms for generalisation, decentralising databases of different vendors or health systems, and incentivizing solutions that improve outcomes over those that do not, the integration of blockchain with AI could help to advance the goal of personalised cardiovascular medicine. . However, such apps are still in their early stages of development, and there are certain worries regarding their implementation. More study is needed in areas such as technological trust, whether rival companies would want this flow of data in practice, remuneration, and ethical issues.
References
- Topol EJ High-performance medicine: the convergence of human and artificial intelligence. Nat. Med 25, 44–56 (2019). [PubMed] [Google Scholar]
- Krittanawong C et al. Deep learning for cardiovascular medicine: a practical primer. Eur. Heart J 40, 2058–2073 (2019). [PMC free article] [PubMed] [Google Scholar]
- Minchole A & Rodriguez B Artificial intelligence for the electrocardiogram. Nat. Med 25, 22–23 (2019). [PubMed] [Google Scholar]
- Loring Z, Mehrotra S & Piccini JP Machine learning in ‘big data’: handle with care. Europace 21,1284–1285 (2019). [PMC free article] [PubMed] [Google Scholar]
- Giordanengoa A Possible usages of smart contracts (blockchain) in healthcare and why no one is using them. Stud. Health Technol. Inform 264, 596–600 (2019). [PubMed] [Google Scholar]
- Mamoshina P et al. Converging blockchain and next-generation artificial intelligence technologies to decentralize and accelerate biomedical research and healthcare. Oncotarget 9, 5665–5690 (2018). [PMC free article] [PubMed] [Google Scholar]
- de Denus S et al. Spironolactone metabolites in TOPCAT — new insights into regional variation. N. Engl. J. Med 376, 1690–1692 (2017). [PMC free article] [PubMed] [Google Scholar]
- Wiggers K PatientSphere uses AI and blockchain to personalize treatment plans. VentureBeat https://venturebeat.com/2018/10/25/patientsphere-uses-ai-and-blockchain-to-personalize-treatment-plans/ (2018). [Google Scholar]
- Popov G The future of artifical intelligence in healthcare! SkyChain https://skychain.global/upload/iblock/89a/wp_english_Newest.pdf (2019). [Google Scholar]
- O’Donoghue O et al. Design choices and trade-offs in health care blockchain implementations: systematic review. J. Med. Internet Res 21, el 2426 (2019). [PMC free article] [PubMed] [Google Scholar]:Articles-PMC8186804
 Previous Post
Previous Post
