Leveraging Narrative Research to Address Healthcare Challenges: Key Applications in Clinical Practice
Leveraging Narrative Research to Address Healthcare Challenges: Key Applications in Clinical Practice
- Home
- Academy
- PhD Research Methodology
- Leveraging Narrative Research to Address Healthcare Challenges
Key Applications in Clinical Practice
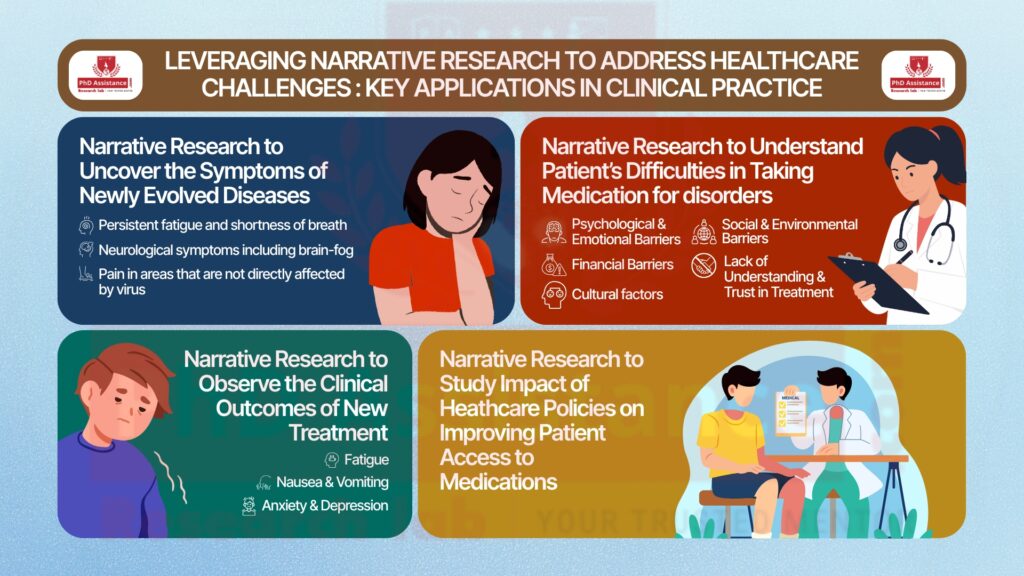
- 1. Narrative Research to uncover the symptoms of newly evolved diseases.
- 2. Narrative Research to Observe the Clinical Outcomes of New Treatment
- 3. Narrative Research to Understand Patients' Difficulties in Taking Medication for Disorders
- 4. Narrative Research to Study the Impact of Healthcare Policies on Improving Patient Access to Medications
- Educational Research
- Exploring Personal Growth and Professional Identity
- Understanding Marginalised Voices
- The Evolution and Historical Development of Narrative Research
- Different Narrative Designs and Their Implications for PhD Research

Recent Post
Introduction
Narrative research is an especially valuable qualitative method that allows researchers to study and understand a person’s lived experiences more deeply. This qualitative research method has a unique lens to study complex healthcare concerns, including chronic disease management, the effectiveness of pharmacological therapies, patient adherence to therapeutic regimens, and the effectiveness of implementation of healthcare policies by examining personal narratives. In this paper, we will provide four important areas in healthcare where narrative research can drive innovation and/or outcomes, enlivened by real-world examples for healthcare researchers.
1. Narrative Research to uncover the symptoms of newly evolved diseases.
Case Example: Narrative Research in COVID-19 Patients to Understand Long-Term Symptoms
With the onset of the COVID-19 pandemic, a newly evolved illness was presented, featuring ever-changing symptoms, even some unknown or poorly understood. As the pandemic progressed, researchers turned to narrative research to find and discover the less obvious symptoms patients experienced, particularly those in patients experiencing long COVID (or post-acute sequelae of SARS-CoV-2 infection, PASC).
Narrative inquiry was utilised in the study by Mandal et al. (2021) to investigate the long-term consequences of COVID-19 in patients who recovered from the acute phase of the illness but suffered from ongoing symptoms. By conducting in-depth interviews with patients, researchers were able to describe and identify symptoms that were not focused on previously, including:
- Persistent fatigue and shortness of breath.
- Neurological symptoms, including brain fog, memory lapses, and difficulty concentrating.
- Emotional distress, including symptoms of anxiety and depression.
- Pain in areas of the body not directly affected by the virus, such as muscle and joint pain.
- Sleep disturbances, reported by a significant number of patients, include difficulty falling asleep and frequent wake-ups throughout the night.
Takeaway for Researchers
The narrative research approach in this situation proved to be valuable for revealing symptoms of COVID-19 that previously not reported and which would begin to address the medical gap in knowledge surrounding an emerging disease. Through patient perspectives and experiences, researchers were able to provide a more detailed view of the disease’s impact to help influence clinical guidelines and healthcare policy.
2. Narrative Research to Observe the Clinical Outcomes of New Treatment
Clinical trials often evaluate the efficacy and safety of new drugs in clinical, controlled experiments. However, narrative research can serve as an additional source of understanding about patients’ experiences (or side effects, benefits or implications) of the drugs during and beyond the treatment process.
Case Example: Narrative Study on New Cancer Drug Therapies
In oncology, new drug therapies often create considerable hope for the possibility of achieving better outcomes for patients. New drugs also may have unpredictable side effects that can influence patients’ quality of life. Narrative research can be especially valuable to investigate both side effects and clinical benefits, provided that it offers depth of understanding from the patients’ perspectives—a key element to evaluate a drug’s overall efficacy.
Barker and Collier (2015) utilized narrative inquiry to examine side effects and clinical gains of new cancer drug therapies. The narrative inquiry focused on patients receiving chemotherapy and immunotherapy which were new to the clinic. The authors utilised narrative inquiry for in-depth interviews with cancer patients to collect data around side effects and benefits considered opaque by traditional clinical trials. The narrative provided the following account:
Side Effects:
- Fatigue
- Nausea and vomiting
- Anxiety and depression
- Hair loss
Clinical benefits:
- Significant reduction in tumour size
- long-term remission
Takeaway for researchers
Quantitative methodology provides insights into haematological and diagnostic parameters such as WBC count, Platelet count, and efficacy parameters. But a qualitative research methodology, such as narrative research, can provide actual clinical outcomes that a person experiences after the treatment. By this, researchers can observe the type and extent of adverse effects in chronic disorders such as cancer, rheumatoid arthritis, and Alzheimer’s disease.
3. Narrative Research to Understand Patients' Difficulties in Taking Medication for Disorders
Adhering to a medication regimen is a perpetual struggle for many patients, in the context of both acute and chronic health conditions. Narrative research offers a rich landscape for examining the social, personal, and psychological factors that influence a patient’s ability to adhere to a prescribed treatment plan, particularly in cases involving complex or chronic conditions.
Case Example: Exploring Medication Adherence Challenges in Patients with Chronic Illnesses
Patients living with chronic disorders (e.g., hypertension, diabetes, chronic pain) often encounter great difficulty in adhering to their prescribed medication regimen. Although the health benefits of adherence to a prescribed medication plan are well-documented, patients frequently encounter barriers to their ability to adhere to their treatment plan, creating added costs to the healthcare system and contributing to poor health outcomes. Narrative research is a very effective vehicle for understanding a patient’s own stories, which showcase the complexities and multitude of things that create the barriers to adherence to a medication regimen.
Hughes and Wong (2018) performed a narrative study on the barriers to medication adherence by individuals with long-term conditions. They conducted qualitative, in-depth interviews of patients diagnosed with chronic conditions, including diabetes, hypertension, and rheumatoid arthritis. Through patient narratives, the researchers were able to draw out multiple barriers to medication adherence:
- Psychological and Emotional Barriers
- Financial Barriers
- Lack of Understanding and Trust in Treatment
- Social and Environmental Barriers
- Cultural Factors
Takeaway for Researchers
Narrative research offers a methodology to understand the complexities of medication adherence than what is offered by quantitative research. By centring on a patient’s voice, researchers can create more useful interventions, better patient education, and therefore improve medication adherence and ultimately, health outcomes for patients with chronic illnesses.
Table 1: Key Applications of Narrative Research in Healthcare
Application Area | Purpose | Case Example | Insights Gained |
Uncover Symptoms of Newly Evolved Diseases | Identify unknown or poorly understood symptoms through patient narratives | COVID-19 Long-Term Symptoms (Mandal et al., 2021) | Persistent fatigue, shortness of breath, neurological issues (brain fog, memory lapses), emotional distress, sleep disturbances |
Observe Clinical Outcomes of New Treatment | Understand real-world side effects and benefits beyond quantitative measures | Cancer Drug Therapies (Barker & Collier, 2015) | Side effects: fatigue, nausea, anxiety; Benefits: tumor size reduction, long-term remission |
Understand Patients’ Difficulties in Medication Adherence | Explore social, psychological, and cultural barriers to treatment compliance | Chronic Illness Medication Adherence (Hughes & Wong, 2018) | Barriers: psychological/emotional, financial, lack of trust, social/environmental, cultural factors |
Study Impact of Healthcare Policies on Access to Medications | Assess how policies affect patient access and affordability | Policy Implementation Studies | Insights into gaps in access, cost-related challenges, and patient/provider experiences |
Example: A researcher might study the narratives of first-year teachers as they transition into the profession. The stories scholars gather from teachers will tell a detailed, textured account of their experiences with their initial struggles, successes, and how they shape their practice over a period. This kind of inquiry offers a solid, novelty factor, and a unique contribution to designing teacher educator programs or other development opportunities (McEwan & Egan, 1995).
4. Narrative Research to Study the Impact of Healthcare Policies on Improving Patient Access to Medications
Healthcare policies play an essential role in determining whether patients will have access to necessary medications. Narrative approaches allow for researching the role of healthcare policies on access to medications and their prices while also incorporating patients and healthcare providers’ lived experiences.
Case Example: The Role of Healthcare Policies in Improving Medication Access in Low-Income Communities
Al Meslamani (2024) conducts a study that considers how healthcare policies related to accessing the healthcare system and medication cost impact medication adherence for low-income populations. More specifically, Al Meslamani highlights how policy interventions (e.g., subsidised medications, reduced complexity of medication regimens, and increased healthcare coverage) help address medication adherence in low-income communities. Al Meslamani (2024) concentrated on barriers to the implementation of the policies (e.g., bureaucracy and difficulty understanding insurance).
While these barriers exist, research shows that policies aimed at reducing the financial costs of taking medications (such as cost-reducing initiatives or price controls) have a significant impact on medication adherence. Efforts to expand healthcare services or simplify treatment regimens can also improve access, but the research indicates that the effect is diluted with inconsistent execution.
Key Findings:
- Economic Barriers: Despite having insurance, the cost of medications is a major barrier. Policies that reduce out-of-pocket costs, like price controls and subsidies, are only one part of the solution.
- Policy Gaps: The differences in policy application are often inequities, particularly in rural parts of the world, that influence access to necessary medications.
- Improved System Access: Policies that promote insurance coverage or support healthcare infrastructure are important to ensure patients can receive both study medications as well as care.
Takeaway for Researchers:
Narrative studies provide direction for framing healthcare policies to impact access to medicine. By focusing on patients’ lived experiences, researchers can identify both barriers to access and policies that facilitate access. Al Meslamani (2024) can now provide evidence to indicate that policies that promote access to medicines and reduce the costs to patients are critical to evidence-based adherence to medications; this evidence will, in turn, support more explicit policy development, especially for vulnerable populations.
Conclusion: The Power of Narrative Research in Healthcare
PhD scholars in the healthcare field can use narrative research as a valuable way to explore complicated problems in clinical practice. By focusing on the patient’s voice and lived experiences, the interpretive framework of narrative research allows scholars to understand complexities that are often overlooked within traditional quantitative methodologies. Narrative research can help scholars to understand the emotional and psychological aspects of chronic illness management, investigate the real-world effects of new drugs, enhance their understanding of lived experiences related to medication adherence, or evaluate the impact of healthcare policies. Narrative research provides a wealth and nuanced depth of insights into understanding healthcare issues from a patient perspective.
As you begin your own narrative research in healthcare, you may consider the following four areas where personal stories may help enhance the depth of your study. Narrative research can provide real-world examples and commitment to lived experiences and is a useful and effective methodology for health scholars to support advancement in healthcare practice, policy and patient outcomes.
References
- Barker, R., & Collier, P. (2015). Narrative inquiry into the clinical outcomes and side effects of new cancer drug therapies. Journal of Oncology Nursing, 42(4), 263-270. https://doi.org/10.1007/jon2015.25
- Hughes, C., & Wong, S. (2018). Barriers to medication adherence in chronic illness: A narrative study. Journal of Health Psychology, 23(6), 723-734. https://doi.org/10.1177/1359105318763889
- Mandal, S., et al. (2021). Exploring long-term symptoms in COVID-19 patients: A narrative research study. The Lancet Public Health, 6(8), e451-e458. https://doi.org/10.1016/j.lancet.2021.06.003
- Al Meslamani, A. Z. (2024). Policy solutions for medication non-adherence: What can governments do? Journal of Health Policy and Management, 45(8), 777-781. https://doi.org/10.1080/14737167.2024.2321242

